Knee Surgery & Rehabilitation
Kneecap (patellar) pain is one of the most common reasons patients seek medical treatment at the Noyes Knee Institute. Kneecap pain is especially concerning in younger individuals who are physically active. Women are at a higher risk than men for developing this problem. Unfortunately, 70-90% of patients will suffer chronic or recurrent problems with kneecap pain.
There are many potential causes of patellar pain, ranging from a traumatic injury to problems with the patient’s anatomy. Many terms have been used to describe this problems:
- Patellofemoral pain syndrome
- Painful patellar syndrome
- Patellofemoral pain
- Runner’s knee
- Jumper’s knee
- Housemaid’s knee
- Anterior knee pain
- Retropatellar pain
- Chondromalacia patella
- Patellofemoral chondromalacia
- Malalignment
- Subluxation
- Dislocation
- Instability
Why Choose NKI for your ACL Reconstruction
The medical staff at the Noyes Knee Institute have decades of experience treating this problem. Our philosophy is to treat (in almost all cases) kneecap pain with conservative treatment first before surgery is considered. Only in cases where this treatment fails to alleviate pain and limitations is surgery recommended.
Frequently Asked Questions
Kneecap Pain What you need to know:
What are the injuries that cause kneecap pain?
- Patellar dislocation or subluxation
- Fracture (bone break)
- Bone bruise
- Tear of the patellar tendon
- Tear of the quadriceps tendon
- Tear of the medial patellofemoral ligaments
- Damage to the articular cartilage (joint lining)
What other conditions cause kneecap pain?
Although some patients have a distinct injury that causes kneecap pain, most do not. There are many other potential causes of this problem, the most common of which are:
- Overuse of the knee joint
- Sudden excessive increase in physical activity level
- Weakness, tightness, or imbalance of the lower leg and hip muscles, including the quadriceps, hamstrings, and iliotibial band
- Prepatellar bursitis
- Pes anserine bursitis
- Chronic patellar subluxation
- Inflamed fat pad
- Patellar tendinitis
- Quadriceps tendinitis
- Chronic generalized synovitis
- Inflamed synovial plica
- Extensor mechanism malalignment
Uncommon Conditions That May Cause Patellar Pain
There are other uncommon causes of patellar pain:
- Prior fracture
- Meniscus tear
- Neuroma
- Chronic instability from ligament tears that were not surgically fixed, especially the posterior cruciate ligament and medial patellofemoral ligament
- Complex regional pain syndrome
- Reflex sympathetic dystrophy
- Rheumatoid arthritis
- Gout
- Septic arthritis
- Pseudogout
- Osteochondritis dissecans
- Osgood-Schlatter’s disease
- Sinding-Larsen-Johansson syndrome
- Patella infera
- Patella alta
- Bone tumor
- Symptomatic bipartite patella
- Severe arthritis between the tibia and femur (tibiofemoral joint) with loss of articular cartilage
- Referred pain from the hip with arthritis
- Referred pain from the sciatic nerve, lumbar disc
- Irritation of the saphenous nerve
How is the cause of patella pain diagnosed?
Because there are many structures involved with the patellofemoral joint, it is important for your physician to determine to the best of his or her ability exactly what is causing your kneecap pain in order to treat the problem efficiently and correctly. While this may seem straightforward, it can be complicated because the pain may be due to different factors.
A diagnosis should indicate all of the problems present, which can only be done after a thorough examination is made of your knee and entire lower limb, including x-rays and magnetic resonance imaging (MRI) if required. At the NKI, we spend a considerable amount of time and obtain all tests required to determine all of the factors that are causing your kneecap problems. You can be assured that our 4-decades of experience in treating all causes of kneecap problems allows us to design a treatment program specific for your problems.
What are the treatment options for kneecap pain?
In our experience, conservative measures such as appropriate exercises, shoe inserts, anti-inflammatory medications, activity modification, weight loss or control, and brace or knee sleeve support frequently alleviate the majority of kneecap pain and instability problems. This is true for both injuries and chronic kneecap problems.
In our Center, every patient meets with our highly experienced physical therapy staff who will design a program of exercises that are “knee friendly” yet effective in gaining strength, endurance, stability, and flexibility. The physical therapist will discuss with you the activities that cause problems and your goals in terms of sports or work requirements. The therapist and physician will watch you walk to determine if your normal “gait” or walking stride needs to be adjusted. The assessment includes examining your feet to determine if a shoe insert or orthotic might be recommended.
Your body weight is an important factor to consider because every pound of body weight is multiplied 3-4 times during daily activities and up to 6-8 times with stairs and squatting activities. In fact, you may not improve with conservative treatment until a normal body weight is achieved. If you have a normal weight, we advise you to be careful to maintain this and it may be necessary to reduce your caloric intake if your activity level is reduced.
How would you treat my teenage athlete who has kneecap pain?
Some of the most frequent patients we see are teenagers with kneecap pain that usually comes on gradually over time, but once it becomes a problem, is difficult to resolve. The dilemma adolescent athletes face who are involved in sports is that there is no true off-season to rest and allow inflammed knee tissues to heal. These athletes either go from one sport to the next all year long, or participate in their single sport the entire year without taking any time off. Some athletes may elect to participate in more than one team in order to be able to travel and receive as much attention as possible from collegiate coaches and recruiters. The constant demands from coaches and parents add to the athlete’s belief that taking time off will result in falling behind others in skill development and talent recognition.
In these athletes, overuse and inflammation of soft tissues is the usual cause of patellar pain. Even if a mild malalignment is found, relieving the stresses on the kneecap and following a careful course of rehabilitation and conservative management will usually be effective in resolving the pain. Both the patient and parents are counseled that rest and time away from the athlete’s sport are necessary to avoid the pain becoming a chronic or recurring problem
One of the most common tissues that remains inflammed is the fat pad. The tissues in the fat pad may swell, which can be seen by the physician. Any pressure applied by the physician on these tissues produces pain. There are also other soft tissues inside the knee that may stay inflammed for long periods of time.
In recurrent overuse cases, the athlete may have to pick one sport or limit certain activities within a sport. Running and jumping activities are particularly problematic. Cross-country running is especially hard on the patella because the knee undergoes excessive twisting and turning as the foot lands on uneven terrain. As the athlete grows, there may be excessive tightness of the hamstrings and quadriceps muscles. Gaining flexibility and strength is very important in these patients
In some patients, kneecap pain from overuse may require months for the symptoms to subside. Only gentle exercises should be done and anti-inflammatory medications may be prescribed. If the patellar joint lining is damaged, the symptoms may persist which may lead to permanent restrictions in sports activities. It frequently takes many months of activity restriction and rehabilitation to decrease kneecap symptoms. Surgery is not advised unless a major anatomic abnormality is found. There is frequently a great deal of frustration that develops by the athlete and parents because there appears to be no quick solution to this problem. Fortunately, with time, the pain and inflammation usually resolve.
Who needs surgery for kneecap pain?
In the event that surgery becomes necessary (if all conservative measures fail to alleviate your pain and/or instability), you can be assured that we have the knowledge, skill, and experience to perform the required procedure using the most advanced techniques available. Our patients begin physical therapy immediately after all operations and that is part of the reason why our complication rates are exceedingly low. Emphasis is placed right away on regaining the normal amount of flexion and extension in your knee (how far it bends and extends), controlling swelling and pain, and “turning on” your leg muscles.
Surgery may be required if all conservative measures do not help relieve patellar pain and a distinct anatomic abnormality is present. We do not perform surgery in patients who do not have any anatomic abnormalities in lower limb alignment, problems with patellar tracking, joint lining damage, or injuries such as fractures that require an operation.
An operation may be necessary to treat for certain injuries, such as patellar fractures that need to be fixed. Patients who have a significant amount of damage to the knee joint lining (articular cartilage) who do not obtain pain relief from the conservative treatment program may also be candidates for surgery. However, they are cautioned that the arthritis-related symptoms may be permanent. Patients who have a painful neuroma or chronically inflammed fat pad or plica syndrome may be candidates for removal of these tissues, but only if conservative treatment fails.
The goals of surgery for patients who have kneecap pain along with instability are to correct any malalignment issues, balance soft tissues, and reconstruct torn or deficient ligaments. There are many different options and the operative plan for each patient is individualized according to the anatomic abnormalities that are present. There are also several types of operations that may be done for patients who have significant damage to the knee joint lining (articular cartilage). These range from removal of loose bodies and fragments of articular cartilage to replacement of all or a portion of the knee.
I am a 35-year old woman and a long-distance runner. My kneecap sometimes moves too much or pops toward the outside portion of my leg – it feels like it is going to dislocate, but it does not. This has happened for years without any problems, but now my kneecap has started to hurt. What should I do?
First, you should see an orthopaedic surgeon and have a comprehensive knee examination and x-rays. You may have some minor damage to the joint lining underneath the patella, but this problem is usually treatable without surgery. You may have a muscle weakness or imbalance that needs to be corrected with physical therapy. A conservative course of treatment may also include shoe inserts or orthotics and anti-inflammatory medications. You should rest your knee and stop running until your pain goes away. A therapist can advise you on exercises you can do to maintain cardiovascular fitness and improve muscle strength and flexibility. Then, when your physician and therapist believe your knee can tolerate more activity, you can slowly resume running.
I have been told I have an inflammed plica, how should this be treated?
An inflammed plica can be difficult to solve if the pain is recurrent and a MRI clearly shows the swollen tissue. We always try conservative treatment first, which includes rest, anti-inflammatory medications, and physical therapy. However, this problem usually requires an operation where the inflammed tissue is removed with an arthroscope.
I have pain in the front part of my knee, just below the kneecap, on each side. What is this and how should it be treated?
One common diagnosis for pain in this area is an inflammed and impinged fat pad, also known as “Hoffa’s syndrome”. Your physician’s examination will show tenderness over the entire fat pad area. You may have an injection test (with Xylocaine) that is also helpful in diagnosing this problem. This may be quite painful and not relieved with conservative treatment. This problem frequently requires an operation to remove the painful fat pad tissue with the use of an arthroscope. Physical therapy is required after surgery and it may take many weeks to recover.
I am 16 years old and run cross-country. My knee has started to hurt. What should I do?
First, try to run shorter distances if your coach will allow. You may ice your knee after you run and take an anti-inflammatory medication such as Aleve. If this does not help, you should stop running and be seen by an orthopaedic surgeon for a complete evaluation. Kneecap pain in teenagers is usually solved with conservative treatment, but it is very helpful to be under the advice of an orthopaedic surgeon and physical therapist to prevent the problem from becoming chronic.
My doctor has told me that I need a lateral release. I have extensor mechanism malalignment. Is this the right operation for my problem?
The answer to this question is usually no. A lateral release should only be done when extreme tightness of the lateral retinacular tissues is detected on the physician’s examination. Otherwise, this operation would not help solve your malalignment problems.
My son, who is 15 years old, dislocated his kneecap a year ago playing soccer. The doctor says he already has some damage to the joint lining under his kneecap. What should we do?
This represents a serious problem for an active teenager. He is too young for surgery. Because damage has already occurred, your son should limit his sports activities to those that are low-impact in order to give his knee as many years as possible before he will have to undergo some type of surgery. Activities such as bicycling and swimming are good to maintain fitness and avoid gaining weight. He can do weight lifting, but should be under the supervision of a physical therapist that can guide him on how to use knee-related weight machines correctly. We recommend a glucosamine-chondroitin sulfate supplement and yearly examinations with an orthopedist to keep track of his knee.
What exactly is the “patellofemoral joint”?
The patellofemoral joint is the portion of the knee where the patella (kneecap) and femur (thigh bone) meet. There are many structures that affect the function of the patellofemoral joint in terms of how the patella tracks and absorbs the forces of weight bearing. These structures are collectively referred to as the “extensor mechanism”:
- Quadriceps muscles (rectus femoris, vastus lateralis, vastus medialis, vastus intermedius)
- Quadriceps tendon
- Patella
- Patellar tendon
- Medial retinaculum
- Lateral retinaculum
- Medial patellofemoral ligament (MPFL)
- Tibial tubercle
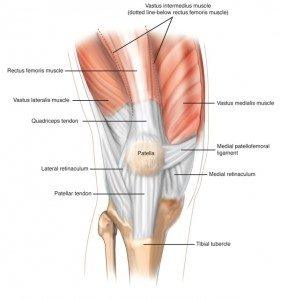
These structures propel the legs forward when you walk, run, or jump. “Extensor mechanism malalignment” is a commonly used phrase by orthopaedic surgeons to describe patellar tracking or instability problems. Patellar stability is the condition in which the kneecap glides normally and stays within the trochlear groove as the knee flexes and extends. An injury, deficiency, or anatomic abnormality of any of the structures listed above may result in patellar pain.
When looking at a leg from the front, the quadriceps muscles and tendon do not form a straight line. They point one way above the patella, and another way below the patella. The quadriceps angle (Q angle) is the angle formed by one line drawn from the pelvis anterior superior iliac spine to the middle of the patella, and a second line drawn from the middle of the patella to the tibial tubercle. The normal Q angle in men ranges from 8-14 degrees. In women, the normal Q angle ranges from 11-20 degrees.
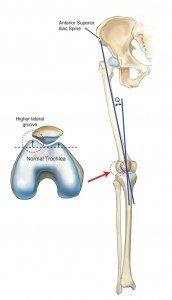
Patella stability is influenced by several factors: the angle of knee flexion, the shape (geometry) of the trochlear groove and lateral femoral condyle, tissues referred to as static patella stabilizers, and tissues called dynamic patella stabilizers.
The static patella stabilizers are the trochlear groove, the MPFL, the patellomeniscal ligament, the patellotibial ligament, the medial retinaculum, and the lateral retinaculum.
The dynamic stabilizers are the quadriceps tendon, patellar tendon, rectus femoris muscle, vastus medialis obliquus muscle, vastus lateralis muscle, and iliotibial band.
An alteration caused by imbalances of these stabilizers may result in patellar maltracking or instability problems, and increase the forces on the kneecap that lead to pain and eventual deterioration of the joint lining.
If you suffer from both kneecap pain and instability, please see the section on Unstable Kneecap (Patella) for more information about instability.
Researchers have recently emphasized the role of the hip muscles in patients with patellar pain and instability. Realize that the hip shares a common bone with the knee – the femur. At the hip joint, the femur connects with the acetabulum of the pelvis and acts as a “ball-and-socket” joint that moves in all directions. At the knee joint, the femur is tightly connected to the tibia through ligaments, tendons, and the joint capsule.
Weakness of the hip muscles (hip abductors and external rotators) may directly impact the knee joint by causing the femur to internally rotate and the knee to go into a knock-knee (valgus) position and the foot to turn outward (pronate). Here is an example of a knock-knee position in a young female athlete who just landed from a jump:
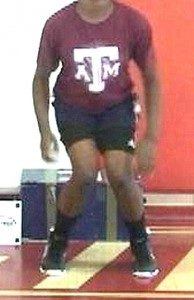
A few studies have shown that patients with kneecap pain and instability have weak hip muscles, but it is unclear if this problem was present before or as a result of the patellar pain.