Knee Surgery & Rehabilitation
Injuries to the posterior cruciate ligament (PCL) are rare, accounting for only about 2-3% of all knee ligament injuries. There is disagreement among physicians over which patients with isolated PCL ruptures (that do not have any other ligament damage) should have surgery and which patients should not have surgery – and for those who need surgery, just how to perform it to achieve the best results. The problem is that these injuries can either not cause many problems, or they can be disabling and cause considerable problems with sports and, in some cases, regular activities of daily living.
E-Book Series PCL Reconstruction
Why Choose NKI for your PCL Reconstruction
“We believe that young active patients who sustain a complete tear to the PCL should be seriously considered for an early reconstruction of the ligament to avoid arthritis which may develop some years in the future. Unfortunately, many patients who injured their PCL a long time ago often develop arthritis and then seek care when it is too late. The goal of treatment in these patients is usually to provide pain-free activities of daily living, which may or may not include surgery. We were the first in the country to develop a very active rehabilitation program after PCL reconstruction, which includes immediately moving the knee and performing exercises which have resulted in one of the lowest complication rates reported in the medical literature. That’s good news for the patients who require surgery. PCL surgery is still developing and newer techniques are being developed every year.”
Frank Noyes, M.D.
President and Medical Director
Frequently Asked Questions
PCL Reconstruction What you need to know:
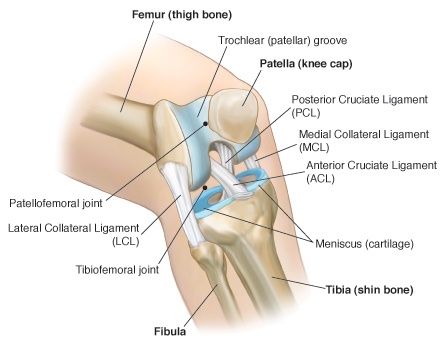
What is the PCL?
The PCL is one of four main ligaments which hold the femur and tibia together. The PCL’s main job is to keep the tibia from falling too far back (posteriorly) from the femur.
How do I know if I’ve torn my PCL?
The most common cause of a PCL injury is a direct blow to the front part of the shinbone (tibia), like hitting the knee on a dashboard in a car. Another way of tearing the PCL comes from the knee “hyperflexing”, or bending too far while the foot is in an awkward position.
Knee “hyperextension”, or the knee straightening past its normal limit, is another way to tear the PCL.
The following symptoms may occur following this injury:
- Swelling
- Loss of motion, or the ability to fully extend and flex the knee
- Pain
When should I see a physician?
If your symptoms last more than two days, you should seek proper medical care; a sports medicine trained physician. If your pain and swelling are severe, seek attention immediately in an emergency room to make sure a fracture has not occurred. Even if you have a partial PCL tear, we recommend that you see a sports medicine physician who will tell you exactly what you are dealing with. Many patients who have a PCL tear also have other damage in their knee – such as another ligament tear or a meniscus tear. These additional injuries may require immediate treatment.
Why should I see a sports medicine-trained orthopaedic surgeon?
The training of an orthopaedic surgeon involves many years of undergraduate, medical school, and residency education. The specialization of sports medicine involves additional training, usually at an educational center where a fellowship year is completed. This involves advanced training in arthroscopic surgery, required in the treatment of most knee, shoulder, ankle, elbow and sports medicine-related injuries. The sports medicine-trained surgeon also has knowledge of specific rehabilitation and muscle performance issues to safely regain function and return patients to athletics. A sports medicine center combines the disciplines of physicians, physical therapists, athletic trainers, and more to totally heal all aspects of an injury.
Will I Need Surgery?
The answer is “yes” if:
The PCL is completely torn and you also have:
- a tear in another ligament (or ligaments), such as the anterior cruciate ligament, medial collateral ligament, lateral collateral ligament, or posterolateral ligament. We recommend reconstruction of all torn or deficient knee ligaments to restore normal stability in the knee joint.
- a tear in your meniscus, especially if your knee locks or catches several times daily
- the desire to return to very strenuous athletics
- frequent instability and giving-way of the knee that formal rehabilitation and other conservative measures cannot alleviate
The answer is “no” if:
- the PCL is only partially torn
- the PCL is completely torn, but you do not have the desire to return to strenuous athletics and you do not have problems with instability with activities of daily living
- severe arthritic damage is present in your knee
Before you can have surgery:
- Knee swelling and pain must be eliminated
- You must go through rehabilitation to strengthen your knee. It is easy to loose muscle very quickly. Rehabilitation focuses on regaining muscle strength in addition to mental preparation for the surgery. The stronger your knee and attitude are before surgery, the better your surgical outcome will be.
What Are My Surgical Options?
At Cincinnati Sportsmedicine, we prefer to use autograft tissue (taken from your own body) for the majority of PCL reconstruction. Our graft of choice is the quadriceps tendon which is implanted using an all-inside technique. The bone portion of the graft is placed on the tibia and the tendon portion of the graft is placed on the femur.
In rare instances in our Center, Achilles tendon allografts (taken from a cadaver donor) may be used for PCL reconstruction. These cases usually involve either sedentary patients or patients with chronic multiple ligament ruptures in whom autograft tissues are not available or feasible to use for surgery. We only use allograft tissues from tissue banks that are certified by the American Association of Tissue Banks and have passed FDA inspection. The allografts are irradiated to kill bacteria and many viruses. The level of irradiation (2.5 megarads) does not harm the biomechanical properties or healing capabilities of the allograft tissues.
What Can I Expect Following My Surgery?
Rehabilitation is an essential element of your recovery. The success of your PCL reconstruction is not only determined by an expert surgeon, but also by following a rigorous rehabilitation program. YOUR SURGERY MAY FAIL IF YOU DO NOT FOLLOW THE RIGHT REHABILITATION PROGRAM.
Our program involves:
- Immediate knee motion and exercises following surgery
- Crutches for about 6 weeks
- Protection against strenuous hamstring exercises for 5 to 6 months
- Running, if desired, 6 months or more after surgery**
- Return to strenuous sports, if desired, 9-12 months after surgery**
**Only if certain muscle strength, ligament function, neuromuscular, and symptom criteria are met. Patients with arthritis are usually advised to return only to light recreational activity to avoid further joint damage.
How do I avoid complications after surgery?
Because patients who have PCL reconstruction often have other ligaments in their knee reconstructed at the same time, complications can arise more frequently than with other knee operations. In our studies of patients who had PCL reconstruction, only 3% required additional surgery for knee motion problems or infection. This low reoperation rate is a result of our immediate knee motion program, which we were the first in the United States to develop and advocate. Following our rehabilitation program is the best way to avoid problems after surgery.
What if after my surgery, I’m still having problems with my knee?
If your knee has pain and swelling and a feeling of instability, your surgery may have failed. PCL reconstruction that fail often do so because of technical errors by the surgeon. Since this is a rare operation, only a few surgeons have the experience and knowledge to perform the surgery correctly AND understand the important elements of rehabilitation in order to prevent postoperative failure. That is why it is essential to seek out a specially trained knee surgeon who has done many PCL reconstruction to perform this operation.
Should I have the surgery repeated?
Patients benefit from having the PCL reconstruction repeated to prevent further damage to the knee joint and increase their level of activity. Although we usually do not recommend in the majority of cases the return to very strenuous activities after revision surgery, most patients can return to an active lifestyle and improve their quality of life. The level of activity a patient can resume is dependent on the amount of arthritis, or joint damage, that exists; the condition of the two menisci; the condition of the other ligaments in the knee; and the postoperative recovery in terms of restoration of muscle strength, balance, coordination, and other factors.
Revision PCL reconstruction is usually performed using the quadriceps tendon autograft in the majority of cases. The exceptions are patients with chronic multiple ligament ruptures in whom autograft tissues are not available or feasible to use for surgery. In these individuals, an Achilles tendon allograft is indicated. Our surgeons are well experienced in using different tissues for revision surgery and have exceptional knowledge in understanding the indications for the various graft options.
It is important to understand that the success rates for PCL revision surgery are somewhat lower than those for first-time PCL reconstruction. There are complicating factors such as weakness to the knee’s “secondary” or supporting tissues which can become stretched or over-worked over time, which are difficult to repair. The patient’s bone at the areas where the graft is attached on the tibia (shin bone) may be soft (called osteopenia) from arthritic damage or repeated injuries and this can affect the ability of the graft to fully incorporate and heal. In many patients, the meniscus has been previously removed and the loss of this important structure can also effect the overall stability that can be achieved through revision surgery.
It is important to understand that the success rates for PCL revision surgery are somewhat lower than those for first-time PCL reconstruction. There are complicating factors such as weakness to the knee’s “secondary” or supporting tissues which can become stretched or over-worked over time, which are difficult to repair. The patient’s bone at the areas where the graft is attached on the tibia (shin bone) may be soft (called osteopenia) from arthritic damage or repeated injuries and this can effect the ability of the graft to fully incorporate and heal. In many patients, the meniscus has been previously removed and the loss of this important structure can also effect the overall stability that can be achieved through revision surgery.