Knee Surgery & Rehabilitation
Partial knee replacement (also called unicompartmental knee replacement) is an operation where just one compartment of the joint is replaced, instead of all 3 compartments that is done in a total knee replacement (TKR, also called total knee arthroplasty). In order to be considered for this operation, the other 2 compartments in the knee joint should have little or no arthritis and a normal amount of joint space. Only the damaged compartment is replaced with metal and plastic; the rest of the healthy bone and surrounding tissue is left alone.
This operation may be thought of as knee "resurfacing" because only the surfaces of the bones are removed and replaced. This is similar to the manner in which a dentist fills a tooth cavity. At our center, the operation is done with the assistance of a robot and advanced software technology that helps the surgeon make very precise calculations and bone cuts in order to achieve the best implant fit possible
E-Book Series Partial Robotic Knee Replacement
PATIENT TESTIMONIALS
One patient's partial knee replacement story
Frequently Asked Questions
Partial Knee Replacement What you need to know:
Who Are Candidates for Partial Knee Replacement?
Patients who are 30-60 years of age (although it can be done in younger or older patients) and who have:
- One area of the knee has significant damage (loss of all cartilage down to bone)
- The other areas (compartments) in the knee joint are normal or nearly normal in terms of the condition of the articular cartilage and joint spaces (< 50% joint narrowing).
- Patients who understand that the overall goal is to buy time before a total knee replacement may be required.
- It is important to understand that if the rest of the knee joint already has some arthritic damage, a TKR will probably be required within 10 years.
- Patients who have severe knee pain or stiffness that limits daily activities such as walking, climbing stairs, and getting in and out of chairs. Pain and swelling may occur while resting, either during the day or at night.
- Patients in whom knee problems do not improve with rest, medications, injections, physical therapy, and weight control.
- Patients who agree that if more arthritis is found during the operation than previously expected, the surgeon may elect to go ahead and perform a total knee replacement instead of a partial replacement.
Who Are NOT Candidates for Partial Knee Replacement?
Patients who have:
- Moderate to severe joint arthritis in another area of the knee joint
- Excessive body weight (body mass index > 32)
- Lower limb malalignment (varus or valgus > 3 degrees) that cannot be corrected at surgery
- Inability to fully straighten the knee
- Ligament instability
- Prior infection
- Inflammatory arthritis
- Diabetes
- Rheumatoid arthritis
- Complex regional pain syndrome
- Knee arthrofibrosis
- Neuromuscular disorders affecting limb control
- Women with osteopenia (soft bone): dexa scan bone mineral density T score >1 or <-1
How is the Operation Done?
Dr. Noyes uses advanced robotic technology to assist in planning and performing the operation. Partial knee replacement is performed with the assistance of the MAKOplasty robotic system. This system uses a highly sophisticated robotic arm (RioTM Robotic Arm Interactive Orthopedic System) and computer software that enhance the precision of the operation. The robotic system and surgeon work together to make accurate calculations before surgery, resect only the smallest amount of bone required, and place the implant components into the knee in a manner that achieves the best fit possible.
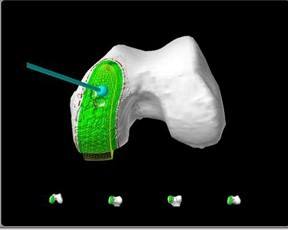
Before the operation, special images are taken of the patient's knee using computed tomography (CT). Several scans are taken of the hip, knee, and ankle joints. The CT scans are fed into a computer and the software program that creates a 3-dimensional (3-D) model of the patient's knee. This model is used to plan the position of the partial knee implants and areas where bone will be removed. The software sets boundaries for the areas in the knee where bone will be taken out in order to prevent cutting outside these areas. The 3-D model is shown to the surgeon on a computer screen, shown below:
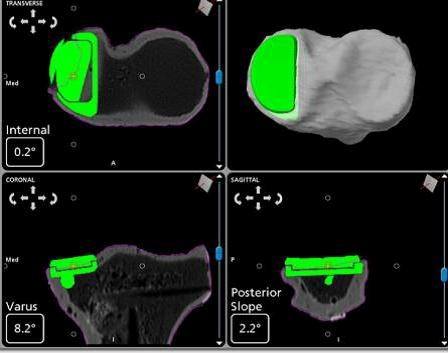
After the patient has been put to sleep, an incision of approximately 4-6 inches is made. Tracking pins are placed into the femur and tibia and a series of bone registration points are collected. These are done in order to set and verify important anatomic landmarks on the tibia and femur, shown below:

The resultant registration of the knee anatomy is sent to the computer and is compared to the previously created 3-D model. The goal is to make sure the 3-D model is indeed extremely accurate in representing the patient's anatomy and that the pre-planned implant position is correct. The patient's knee is taken through several cycles of flexion and extension that allows the surgeon to see the position of the simulated position of the implant components as the knee is moved.
Next, the surgeon removes the damaged articular cartilage surfaces and a small amount of bone. A burr located at the end of the robotic arm is used by the surgeon to remove the amount of bone according to the boundaries previously set by the software from the 3-D model. As the surgeon removes bone, he or she watches the process on a computer screen, shown below:
In the medial unicompartmental procedure, the removed cartilage and bone are replaced with metal and polyethylene components that recreate the surface of the joint.
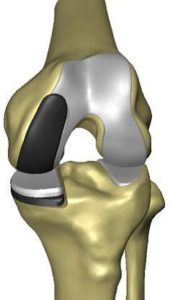
In the patellofemoral procedure, the patella is resurfaced with a plastic button and the front of the femur is resurfaced with a chrome cap.
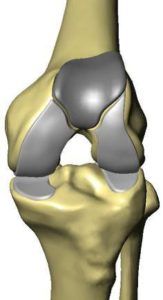
The implants are placed into the knee and images appear on the computer screen, showing the placement and overlapping of the implants as the knee is moved throughout flexion and extension. After the surgeon has accepted the implant position, both of the components are cemented in place. The knee is taken once more through its range of motion. The surgeon verifies the alignment and positioning of the implants.
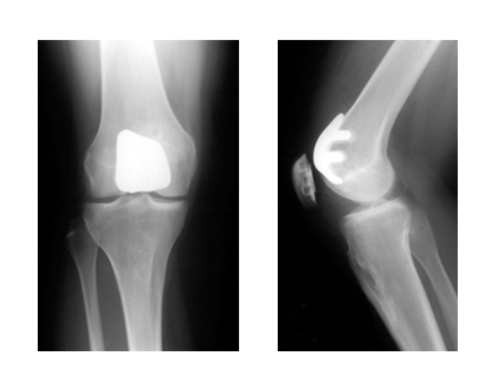
Below is are x-rays of a medial partial knee replacement:
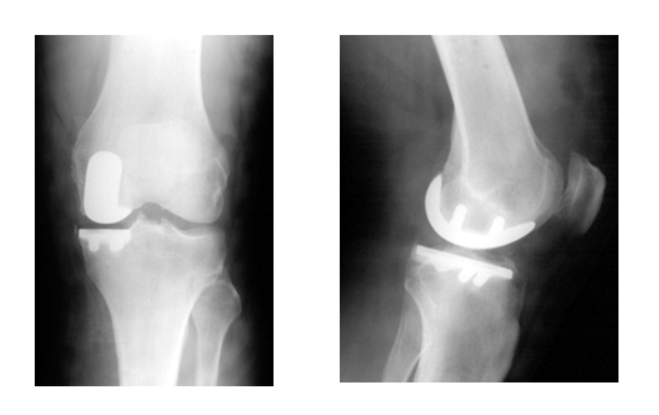
Below is an x-ray of a patellofemoral knee replacement:
What Are the Potential Complications?
The potential complications of partial knee replacement are rare, but include infection, blood clots, implant problems such as loosening or failure requiring revision surgery, neurovascular injury, metal allergy, continued pain, inability to regain knee motion, and other general risks of surgery.
Some surgeons recommend after a partial knee replacement that the patient should receive antibiotics the day before and after any future dental procedures, dental cleaning, or operations. This is because there is a rare risk of bacteria in the blood stream "seeding" to the metal implant.
What is the Postoperative Rehabilitation Program After Partial Knee Replacement?
At the Noyes Knee Institute, most patients are able to walk without a cane or crutches within approximately 3-4 weeks after surgery. The majority can return to their daily activities within 4-6 weeks. Our formal postoperative physical therapy program lasts for 3 months, but most of the exercises are done at home or a fitness facility.
Light, low-impact activities such as walking, swimming, golfing, light hiking, and bicycling can often be performed by 2-3 months after partial knee replacement. However, running and high-impact athletic or occupational activities are not advised and, in fact, should be avoided. This is because the implant has a limited lifespan (approximately 15-20 years) and high impact forces will shorten this timeframe because they may speed up normal wear and cause the knee replacement to loosen and become painful. With appropriate activity modification and weight control, knee replacements may last for many years.
Click here to see our postoperative rehabilitation program.
What Are the Expected Results of Partial Knee Replacement?
Studies published within the last 10 years have shown acceptable survival rates (meaning the knee is still doing well) for medial unicompartment knee replacements. High success rates have been reported with the Oxford Partial Knee (Biomet, USA), with survivorship rates ranging from 85% to 96% at 10 years after surgery and from 83% to 92% at 15 years after surgery. Products from Zimmer, Inc. (Miller-Galante and the Unicompartmental High Flex Knee System) have also very good survivorship rates that range from 70% to 96% at 15 years after surgery.
Studies conducted to date on patellofemoral knee replacement procedures have demonstrated greater variation in long-term survivorship rates. Most short-term (5 years after surgery) survivorship rates of second and third-generation prostheses are excellent, ranging from 77% to 100%. Ten-year rates reported in 4 studies ranged from 59% to 93%. The problems in many of these studies were related to patient selection criteria, including use of patellofemoral replacements in patients who had arthritis in other compartments of their knee, advanced age, and high body weight.
Nutrition Concerns for Patient Undergoing Partial or Total Knee Replacement
Strong Advice for All My Patients by Frank R. Noyes, MD
ALBUMIN is a very important protein in your blood stream that is a key factor in your ability to heal after surgery. About one-third of patients do not have completely balanced diets including meats, eggs, vegetables, and vitamins. Before surgery, we will order an albumin test to make sure your levels are adequate and advise if you need added protein supplementation.
I want my patients undergoing major surgery to supplement their normal diet with added proteins and amino acids. There are many good preparations from GNC stores and online. GNC AMP Wheybolic is one product that provides 40G of protein in 2 scoops and is low in carbohydrates that limits calorie intake. There are other forms of protein at your grocery or pharmacy store. Again, select a high protein, low calorie product. A protein shake with yogurt and blueberries every day is ideal. Do not use if you have kidney disease because the added protein requires good kidney function and hydration. If you are lactose intolerant, try a plant-based product. Start your protein supplements 4 weeks before and continue 8 weeks after surgery.
Yogurt or probiotic products are also recommended for 4 weeks before surgery because you will receive high doses of antibiotics and this helps prevent GI problems after surgery.
Gamma Globulin is also a protein in your bloodstream that is very important to fight infection and prevent infection. It is rare to have low levels; however, you will be tested before surgery to make sure you are protected.
Multivitamins that include good doses of Vitamin D and C and others are important. Most Americans have adequate levels; however, I still recommended a daily multivitamin 8 weeks before and after major surgery.
Vitamin D deficiency is more common in America and most PCPs will test their patients for this at some time. If you are not routinely exposed to sunlight or have a darker complexion, you should be tested because Vitamin D is absorbed through the skin.
Women with any family history of low bone density or bone mass, or over 50 years of age, should have a Dexascan to make sure their bones are healthy and to rule out osteoporosis. This is important because a total knee replacement must be anchored onto good strong bones at the knee joint. Vitamin D and calcium supplementation is important for patients with decreased bone density.
If you are over 50, please have your colon scoped before a knee replacement to avoid this procedure in the early years after surgery. Also, make sure you have no infection in your mouth and that your teeth and gums are in good shape. Any urinary risk factors such as recurrent infection or difficulty voiding require treatment before surgery.
Iron deficiency anemia is important to exclude and you will be tested for your hemoglobin and hematocrit which are measures of your red blood cells. A deficiency may be a reason to cancel surgery because you must have adequate red blood cell levels for surgery and to avoid a blood transfusion.
Diabetics is an added risk factor for surgery and it is highly important that your A1C be normal and not elevated, otherwise, surgery will be canceled.
Excessive body weight is another risk factor for surgery problems and it is important that you achieve a balanced diet and healthy weight. Often, surgery will be postponed to allow time for appropriate weight loss.